By Kei Emmanuel Duku
For a mother or husband in South Sudan, the geography of survival is a cruel map. If your child or spouse has cancer, your life is suddenly divided into three directions: a flight you cannot afford to India, a grueling bus ride to Kampala, or a quiet, agonizing death at home.
In a country of nearly 20 million people, there is no national cancer center and not a single homegrown adult oncologist. Here, the “silent killer” is louder than the sound of gunfire. For families like those of little Evan Gordon and Elizabeth Ayala Wodwa, the lack of a local cure is the ultimate insecurity.
Evan Gordon is only six years old, but he has already faced a war inside his own body. His mother, a single parent, has raised him alone since he was six months old, after his father developed kidney failure. Her life was normal until July 24, when Evan developed a fever that refused to break for a month.
“I went from hospital to hospital for a month,” his mother recalls. “Doctors kept telling me it was just anemia.”
Anemia is a condition where the body lacks enough healthy red blood cells to carry oxygen. However, Evan’s condition was far more threatening. It was only when his mother met Dr. Joseph Gordon that the truth came out; he was diagnosed with Acute Myeloid Leukemia (AML).
AML is a very fast-growing and aggressive type of blood cancer. Because South Sudan lacked the facilities to treat him, Evan was rushed to Kampala, Uganda. For four months, the toddler endured chemotherapy—a harsh treatment using powerful chemicals to kill cancer cells.
“If my child is alive today, it is because of Dr. Gordon,” his mother says. But while Evan is currently in P1 and showing no symptoms, a dark cloud hangs over them. “My worry is if the disease comes back. They told me he would need a bone marrow transplant—where healthy stem cells are put into the body—and that happens in India. I am a single mother. I cannot afford India.”

Dr. Gordon warns that because AML is so aggressive, there is always a risk it could recur, or come back. “If it returns, the only option is that transplant. But we are keeping our fingers crossed.”
While Evan’s mother prays for the future, Bak is living through a present-day nightmare. His wife, Elizabeth Ayala Wodwa, was diagnosed with throat cancer in 2024. The tumor grew so large it caused a complete blockage.
“She could not swallow anything. She had to feed using a tube,” Bak explains. “Without it, she could not survive.”
To save Elizabeth, Bak had to do the impossible: raise enough money to fly to Sabri Hospital in India. They spent seven months in India, exhausting their savings on chemotherapy and radiotherapy-a treatment that uses high-energy beams, like X-rays, to destroy tumors.
They were sent back to Juba when the money ran out, but Elizabeth’s condition worsened. Her feeding tube failed. Desperate, Bak lobbied friends and South Sudanese in the diaspora for more funds. They returned to India in October 2024 for robotic surgery, a precise operation where a doctor uses a computer-controlled robot to remove the diseased throat.
“That surgery rescued my wife,” Bak says. “But now, doctors recommend immunotherapy—a treatment that boosts the body’s natural immune system to fight cancer cells. Because of our money problems, we cannot continue. I am not even working.”
Bak’s voice cracks as he describes the psychological toll. “I am more affected than her. She cries all night because of the pain. If I don’t have the chemical medication—the strong painkillers—she cannot stop crying.”
Frustrated, Elizabeth’s husband described cancer as a major health insecurity in South Sudan, “more than the bullet of a gun.”
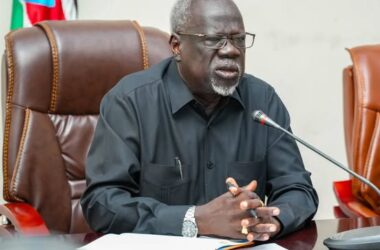
As these families face financial ruin, Professor John Akech, Vice Chancellor of the University of Juba, is sounding the alarm on the systemic failure that leaves patients with no recourse. He argues that cancer treatment is so expensive it cannot be managed alone, and that the country must rethink its entire health economy.
“I would like to remind us that the health system and health sector is classed as an economy of uncertainty,” Prof. Akech stated. “Anyone of us can be ill anytime with any kind of illness, including cancer. Cancer can only be tackled by using an insurance system for our health, the same as we need insurance for our cars.”
Prof. Akech points out that the current “out-of-pocket” system is a trap for the majority of South Sudanese who are hit with massive hospital bills they are not ready for. He believes the solution is simple and immediate: a collective insurance fund.
“First of all, insure everyone in the government. Deduct a small amount of money from everyone, whether in the private sector, NGOs, or government sector, and put that aside,” he explained. “That money stays there because we cannot all be ill at the same time. It is a matter of probability. One or two of us will be ill, and it means that the little contribution we all make will treat somebody. Tomorrow could be our chance, and the day after could be our child’s chance. You never know.”
Beyond the money, Prof. Akech noted that such a fund could pay for life-saving equipment and ensure doctors are well-paid enough to stay awake at night to care for the sick. He used the platform to call for urgent political action to bring modern cancer tools to Juba.
“Our government should accelerate the joining of the International Atomic Energy Agency,” he said. “They can help the country technically establish a cancer center. I also call for our country to join the Convention on the Physical Protection of Nuclear Materials and expedite the establishment of nuclear regulatory authorities.”
Prof. Akech emphasized that nuclear medicine—the use of radioactive substances to see inside the body and kill cancer cells—is one of the most vital tools for controlling the disease.
Adding his voice to the urgency, Dr. Humphrey Karamagi, the World Health Organization (WHO) Representative for South Sudan, explained that the human impact of cancer is a human rights and development issue. He noted that across the WHO Africa region, more than one million people are diagnosed with cancer annually.
“Every cancer journey is different, and we must ensure that no one faces cancer alone. Every person has the right to prevention, early detection, treatment and dignified care when they are facing cancer,” Dr. Karamagi stated.
In South Sudan, estimates suggest cancer causes 7% of all deaths. The drivers are primarily breast and cervical cancers, followed by prostate, liver, and colorectal cancers. Esophageal cancer ranks sixth and is quite common among the South Sudanese population.
Dr. Karamagi warns that cancer treatment is a catastrophic financial strain that weakens an already fragile health system. “Managing cancer is a chronic event; it’s not like malaria, where you give tablets and the person gets better. It drains these resources from other conditions.”
He noted that in South Sudan, most patients are diagnosed late and often based on clinical presentation alone. The situation is challenging without laboratory testing equipment, which hinders the health expert’s ability to respond in time.
The WHO expert painted a tragic picture of the country’s current gaps: “We end up with situations where somebody is picked up with a stage 1 survival of cancer, and they still die, which is quite tragic, because that is something which is easy to manage.”
Looking toward the future, Dr. Karamagi emphasized the need for a national cancer registry to track the disease and the implementation of palliative care—specialized care for terminal patients to ensure people can “exit with dignity.”
Addressing these gaps, Sarah Cleto Rial, the South Sudan Minister of Health, noted that while the country is without a formal cancer registry, international estimates highlight the urgent need for action. She emphasized that cancer impacts not only health but also the social and economic fabric of communities, with families bearing much of the burden.
“They become the health workers providing the health services for their loved ones,” Minister Rial explained. “Our health care system faces many challenges, including limited resources and infrastructure.” She noted that the health budget is annually impacted, with only 1.3 percent allocated for the health sector.
The Minister highlighted the difficult trade-offs the government must make. “We’ve been asking and advocating for the increase of the budget because health is a national security matter, although of recent we have to take difficult decisions to reduce the budget to support many of the health facilities.
She stated that under the health sector transformation project, about 85% of the health budget comes from donors, despite the fact the government is supposed to meet 50% of its health care costs. “We are offering less than 2%, and this has been affecting our health services.”
Despite the reduction in donor funds and the impact of inflation, Minister Rial remains optimistic, urging South Sudanese not to be hopeless. “The government is focusing on important health service delivery affecting the population, and one of them is this cancer.”
She detailed the ministry’s concrete steps to fight back, stating that a cancer department has been developed and a protocol for a baseline assessment to identify gaps is soon to be established.
According to the Minister, the government’s strategy includes focusing on Non-Communicable Diseases (NCDs) like cancer and seeking technical support for a cancer control unit. “We are exploring the establishment of cancer treatment facilities, beginning with an Oncology Department at Juba Teaching Hospital and progressing towards a comprehensive cancer center.”
Minister Rial also acknowledged the tireless work of civil society. “The Cancer Network of South Sudan is not sleeping. They are engaged with organizations including the African Cancer Registry Network and the International Agency for Research on Cancer. We are expecting these organizations to visit South Sudan to help establish the first cancer registry.”
She concluded with a call to unity. “I call upon our partners, the NGOs, the community leaders, and the business sectors to join us in this mission. Together we can strengthen our response to cancer and improve outcomes for all.”
Until the insurance systems and centers proposed by Prof. Akech and the Ministry become a reality, the choice for the people of Juba remains the same.
“I managed to take my wife to India because of my friends and colleagues,” Bak says, looking at Elizabeth. “We shouldn’t have to beg for a life. A country of 20 million people cannot lack the care that rescues its own people.”